Blog
Symptoms of hip or knee osteoarthritis can include:
Pain and/or stiffness in and around the joint with the following:
- walking, standing and stair climbing.
- getting moving in the morning.
- trying to move a joint toward its end of range.
What is osteoarthritis:
Osteoarthritis is characterised by changes such as damage to joint cartilage, bony spurs around the edge of a joint and deterioration of ligaments and tendons (connective tissue).
What causes knee or hip osteoarthritis?
Osteoarthritis has long been considered a 'wear and tear' disorder but this isn't as accurate as we may have thought. Elite athletes in impact sports have a greater chance of developing hip or knee osteoarthritis but it doesn't necessarily cause it; many athletes still don't develop osteoarthritis any quicker than the rest of the population. Despite this, people that exercise and aren't elite sportspeople actually have a reduced likelihood of developing arthritis. It's not known whether the body learns to adapt to the load associated with recreational exercise or whether it is the more general beneficial effects of exercise that have a preventative effect. Another factor consistently shown to put people at a higher risk of hip and knee osteoarthritis is obesity. It is believed that the combination of increased weight as well as inflammation in the body can put the person at greater risk of hip or knee osteoarthritis.
What do I do if I have knee or hip osteoarthritis?
People often report they have stopped their exercises and activity due to joint pain, but sometimes that isn't the best thing to do. We know that recreational exercise can reduce the likelihood of arthritis and being overweight or obese consistently shows an increased rate of hip and knee osteoarthritis. Arthritis Australia makes a very good point - "Who should Exercise?" "Everyone with or without arthritis should be doing regular, appropriate exercise. The important thing is to choose the activities that best suit your condition, health and lifestyle." Increasing leg strength and decreasing weight have consistently been shown to improve the symptoms of hip and knee osteoarthritis. A recent program in Denmark has shown that education as well as regular exercise focused on strength and control significantly improved symptoms. The good news is, by reading this, you've already started the education part!
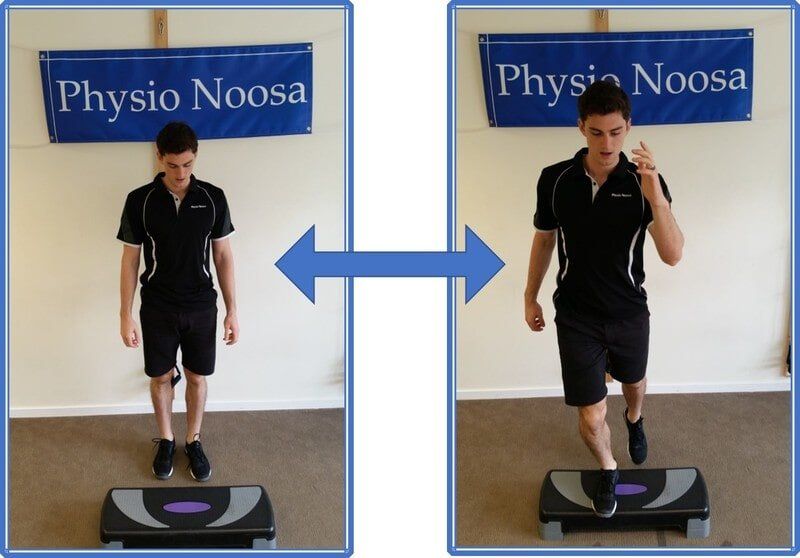
People can find it difficult to know what appropriate exercise is and how much is needed. It's important that you feel empowered to exercise and can be re-assured that you aren't doing any further damage. Physiotherapists and Exercise Physiologists are trained to help you find a way to exercise that works for you. There may be extra benefit from doing exercises that improve the control of your leg and also developing strength in your thigh muscles.
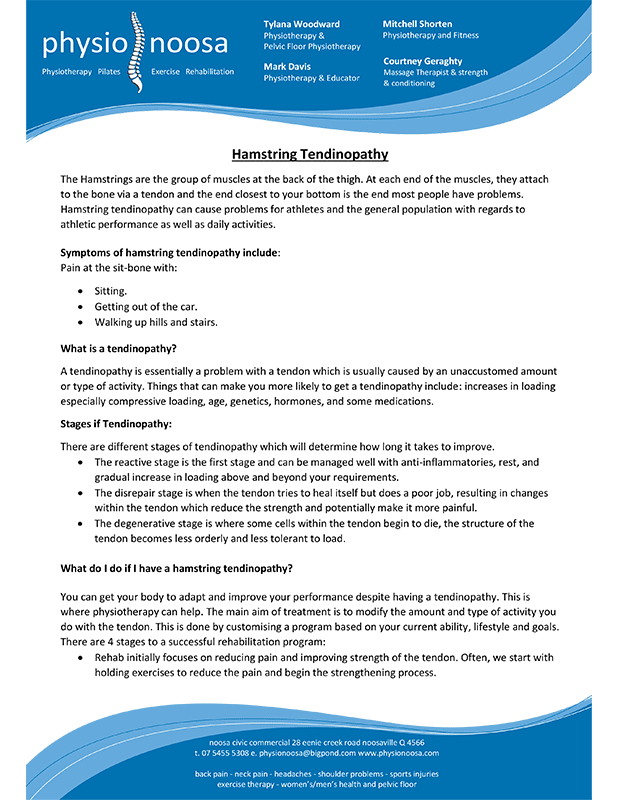
Proximal Hamstring Tendinopathy
The Hamstrings are the group of muscles at the back of the thigh. At each end of the muscles, they attach to the bone via a tendon and the end closest to your bottom is the end most people have problems. Hamstring tendinopathy can cause problems for athletes and the general population with regard to athletic performance as well as daily activities.
Symptoms of hamstring tendinopathy include:
Pain at the sit-bone with:
- Sitting
- Getting out of the car
- Walking up hills and stairs
What is a tendinopathy?
A tendinopathy is essentially a problem with a tendon which is usually caused by an unaccustomed amount or type of activity. Things that can make you more likely to get a tendinopathy include: increases in loading especially compressive loading, age, genetics, hormones, and some medications.
Stages of Tendinopathy:
There are different stages of tendinopathy which will determine how long it takes to improve.
- The reactive stage is the first stage and can be managed well with anti-inflammatories, rest, and gradual increase in loading above and beyond your requirements
- The disrepair stage is when the tendon tries to heal itself but does a poor job, resulting in changes within the tendon which reduce the strength and potentially make it more painful
- The degenerative stage is where some cells within the tendon begin to die, the structure of the tendon becomes less orderly and less tolerant to load.
What do I do if I have a hamstring tendinopathy?
You can get your body to adapt and improve your performance despite having a tendinopathy. This is where physiotherapy can help. The main aim of treatment is to modify the amount and type of activity you do with the tendon. This is done by customising a program based on your current ability, lifestyle and goals. There are 4 stages to a successful rehabilitation program:
- Rehab initially focuses on reducing pain and improving strength of the tendon. Often, we start with holding exercises to reduce the pain and begin the strengthening process.
- The next stage is to progress into slow repetitions through range with increasing loads.
- Your program then progresses into activities that you would like to do, developing strength and speed as required for what you need to do.
- Finally, adding speed to increase stiffness and elastic properties if it's required
Passive treatments such as injections, medications and dry needling may offer some relief but do not help the tendon adapt in the long term. In contrast, active approaches that involve progressive loading such as the program mentioned above have good long term outcomes, especially if rehab is continued after your pain subsides and you can perform the tasks required.
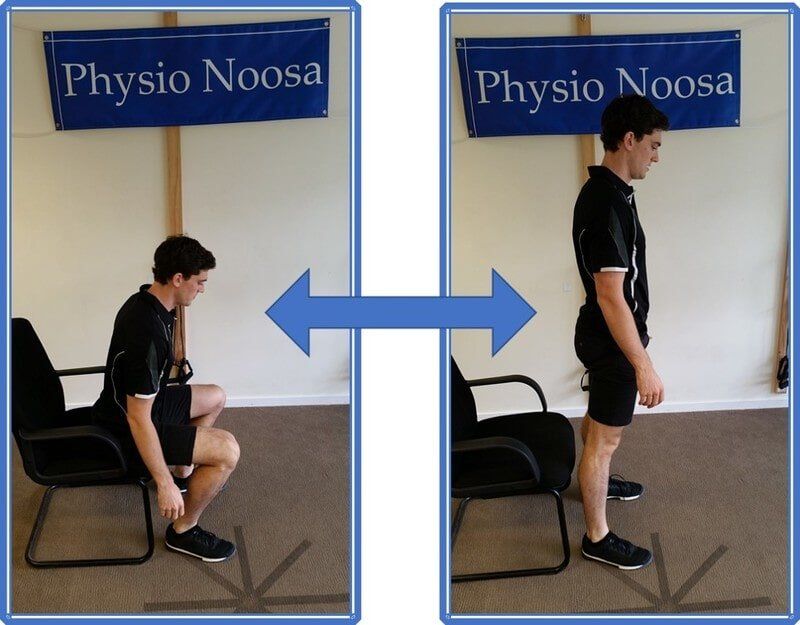
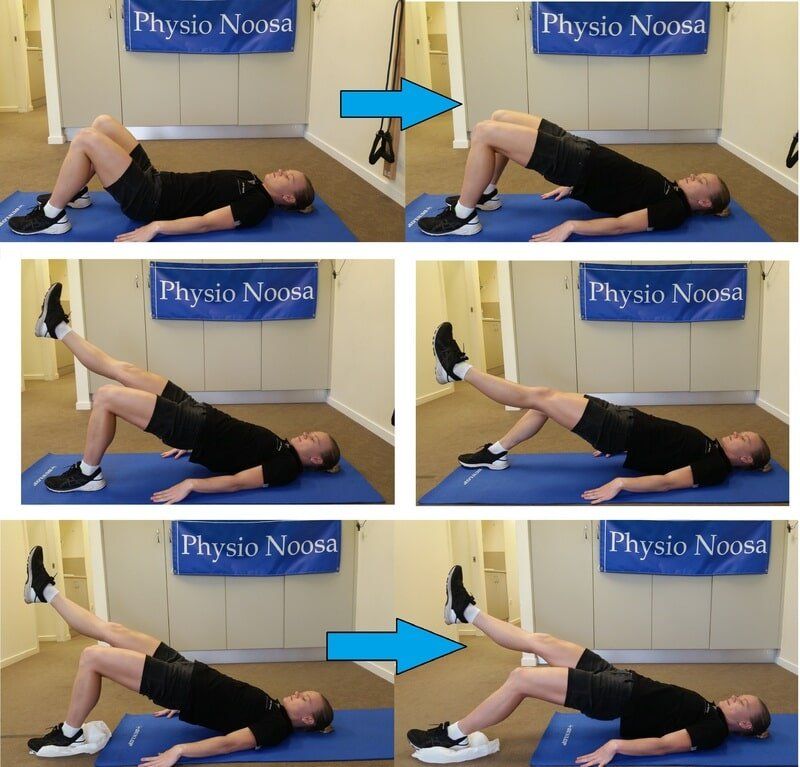
Check out the pictures of Courtney, our Massage Therapist and Strength and Conditioning guru, performing some typical exercises for hamstring tendinopathy rehabilitation.
If you have any of the symptoms mentioned above, come in to get a customised program to get your hamstring feeling great again.
Authors: Tylana Woodward, Mark Davis and Mitchell Shorten.
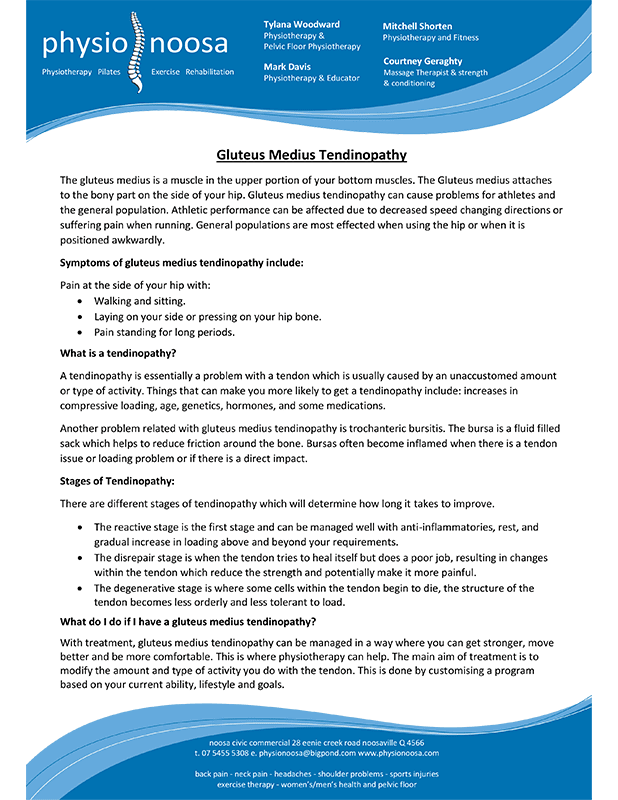
Gluteus Medius Tendinopathy
The gluteus medius is a muscle in the upper portion of your bottom muscles. The Gluteus medius attaches to the bony part on the side of your hip. Gluteus medius tendinopathy can cause problems for athletes and the general population. Athletic performance can be affected due to decreased speed changing directions or suffering pain when running. General populations are most effected when using the hip or when it is positioned awkwardly.
Symptoms of gluteus medius tendinopathy include:
Pain at the side of your hip with:
- Walking and sitting
- Laying on your side or pressing on your hip bone
- Pain standing for long periods
What is a tendinopathy?
A tendinopathy is essentially a problem with a tendon which is usually caused by an unaccustomed amount or type of activity. Things that can make you more likely to get a tendinopathy include: increases in compressive loading, age, genetics, hormones, and some medications.
Another problem related with gluteus medius tendinopathy is trochanteric bursitis. The bursa is a fluid filled sack which helps to reduce friction around the bone. Bursas often become inflamed when there is a tendon issue or loading problem or if there is a direct impact.
Stages of Tendinopathy:
There are different stages of tendinopathy which will determine how long it takes to improve.
- The reactive stage is the first stage and can be managed well with anti-inflammatories, rest, and gradual increase in loading above and beyond your requirements.
- The disrepair stage is when the tendon tries to heal itself but does a poor job, resulting in changes within the tendon which reduce the strength and potentially make it more painful
- The degenerative stage is where some cells within the tendon begin to die, the structure of the tendon becomes less orderly and less tolerant to load.
What do I do if I have a gluteus medius tendinopathy?
With treatment, gluteus medius tendinopathy can be managed in a way where you can get stronger, move better and be more comfortable. This is where physiotherapy can help. The main aim of treatment is to modify the amount and type of activity you do with the tendon. This is done by customising a program based on your current ability, lifestyle and goals. There are 3 stages to a successful rehabilitation program for gluteus medius tendinopathy:
- Rehab initially focuses on reducing pain through education regarding provocative activities and improving strength of the tendon. Often, we start with holding exercises to reduce the pain and begin the strengthening process.
- The next stage is to progress into slow repetitions through range with increasing loads.
- Your program then progresses into activities that you would like to do, developing strength and speed as required for what you need to do.
Passive treatments such as injections, medications and dry needling may offer some relief but do not help the tendon adapt in the long term. In contrast, active approaches that involve progressive loading such as the program mentioned above have good long term outcomes, especially if rehab is continued after your pain subsides and you can perform the tasks required.
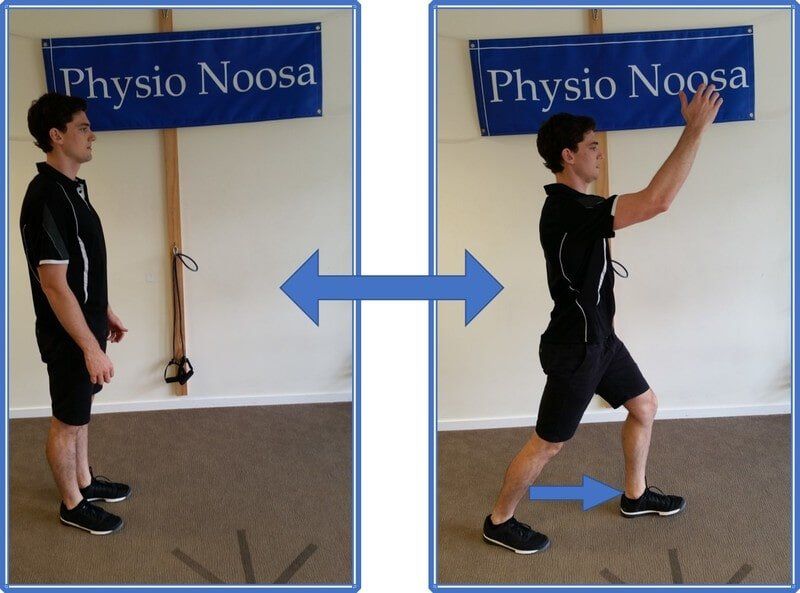
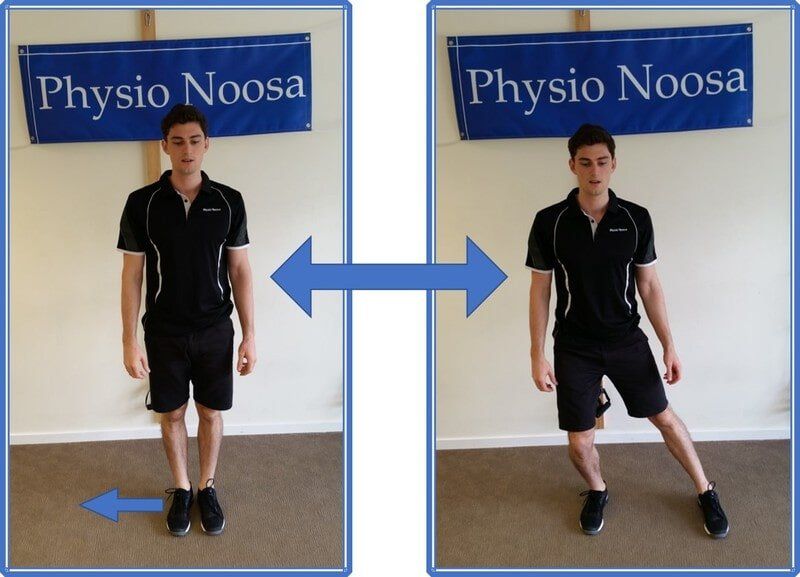
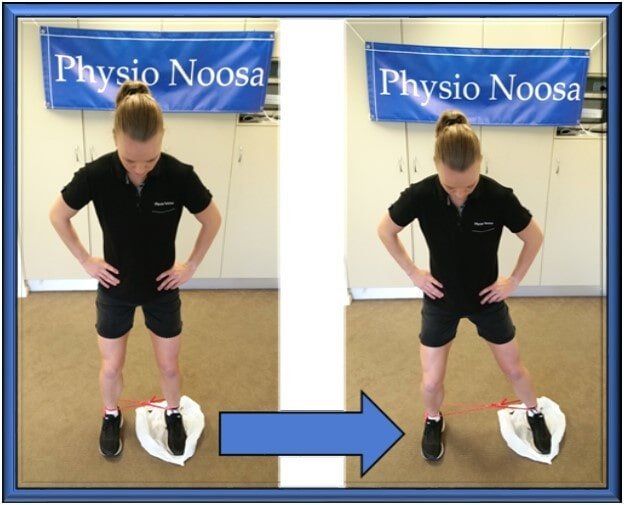
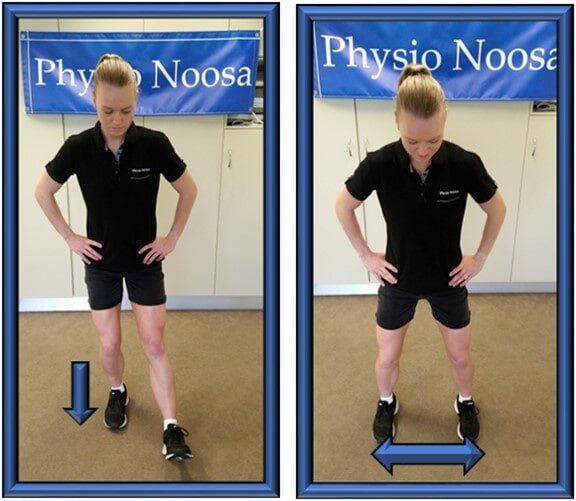
Check out the pictures of Courtney, our Massage Therapist and Strength and Conditioning guru, performing some typical exercises for gluteus medius tendinopathy rehabilitation
If you have any of the symptoms mentioned above, come in to get a customised program to get your hip and glutes feeling great again.
Authors: Tylana Woodward, Mark Davis and Mitchell Shorten.
Why Does It Hurt?
Pain was once thought to be a very basic sense; something damaged you and you would feel pain. We now know that pain is a very complicated response to things that happen in your body and mind.
What is pain?
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage (International Association for the Study of Pain). When you feel pain, it is always real, no matter what is causing it.
What causes pain?
Pain is your brain's best guess at what you need to feel in order to protect your body. You have nerves in your body designed to identify if there is something wrong and these nerves will send a small electrical signal to your brain. Your brain analyses this signal and all sorts of information such as memories, beliefs, emotions, your current level of danger and what you see hear and smell in your environment. Your brain will then decide whether there is actual or the potential for tissue damage. Having pain for a few weeks after an injury is normal, it's the way your body protects itself from further injury.
If you are still experiencing significant pain once your injury has healed, we say this is persistent pain. Usually we would expect things to heal between a couple of weeks and a couple of months, so anything beyond that we would say it is persisting.
What makes pain persist?
Your body and brain have evolved to protect itself at all costs. We know that after a few months of pain persisting, your body will become more efficient at producing pain, which in other words is your body becoming more sensitive to pain! Cells in your spinal cord and brain change to become more responsive, this gives you an increased 'buffer' between when you feel pain and when tissue damage will occur.
Not everything you perceive is real and exactly what you think it is. Think of visual illusions, even though you know they are an illusion, your brain will show you what it thinks is most beneficial. The same thing can happen with pain; regardless of what your body is sensing, your mind can change that if it thinks it will be beneficial. If you are fearful or worried about using a body part after an injury, that can make the pain worse because your brain will take these emotions into account when deciding if it is in danger.
What should I do if I have persistent pain?
There are many ways to treat persistent pain and it's all to do with re-training your pain system. The more you understand about how pain works, the more you will understand that pain and injury are often quite different things.
The good news is, you've already made a start at learning how pain works and what to do about it. Once you understand how pain works, you can start to do a little more than you normally do and gradually build up. Movement and activity is a great way to gradually re-train your pain system and modify how your brain responds to what you do. There are different ways to build up and our Physiotherapists can help you do that. Initially it's a good idea to focus more on the things you can do and try not to focus too much attention to your pain. Trusting that your body can adapt and get used to activities if you give it time is a great mindset to have. Through your journey with persistent pain there will almost certainly be ups and downs and it's important to remember that the pain is protecting you, not telling you that you have damaged yourself.
Sometimes it's useful to discuss things that have affected you in the past because memories and emotions can sometimes be enough to trigger your pain system. It's important to be aware of this so that you know that when your pain flares up, it isn't necessarily because of damage to the system. Having pain like this is quite common and doesn't make it any less real, it still just means that you need to re-train your pain system to be less reactive.
The Ins And Outs Of Incontinence
What is Incontinence?
Incontinence is the involuntary/accidental loss of urine or faeces that becomes a social or hygienic problem. Incontinence affects greater than 850 000 adult Australian men and women. 38% of Australian adults report experiencing incontinence but 62% of those people have not spoken to a healthcare professional about it. Urinary incontinence is not a normal part of ageing or a consequence of giving birth, however, is more common and severe in the elderly. Incontinence has a large effect on emotional and psychological wellbeing. Quality of life and the ability to participate in normal daily activities is largely impacted on.
What causes incontinence?
There are a range of factors that contribute to incontinence including pregnancy, childbirth, constipation, prostate problems, immobility, musculoskeletal, neurological, cognitive problems, surgical procedures and health and lifestyle factors.
Incontinence is not a normal part of ageing, nor a consequence of pregnancy, despite 63% of people believing this to be the case. This stigma and perception that incontinence is normal largely contributes to people not seeking help. However, incontinence can be treated, managed and in many cases also cured.
Types of Incontinence
You may have one of the following or a combination of both called mixed incontinence.
Stress Incontinence
- Occurs with an increase in intra-abdominal pressure such as a laugh, cough, sneeze, run, jump, hop or lifting.
- Other contributing factors include diabetes, chronic cough (linked with asthma, smoking or bronchitis), constipation, straining, obesity and abdominal and pelvic surgeries.
- Weakness of the pelvic floor muscles occurs, which results in the bladder and urethra not being supported well enough.
- When pressure on this area occurs, pelvic structures don’t have enough support by the surrounding pelvic floor muscles and leakage occurs.
- Stress incontinence is involuntary, instantaneous and usually without warning.
Urge Incontinence: Overactive Bladder
- Is the sudden and overwhelming urge to go, with the inability to defer past the initial urge.
- This strong urge is often due to involuntary contractions, or overactivity of the bladder muscle (Detrusor) and ‘The first need to go is often the last’.
- Urge incontinence can occur because of overactivity of the Detrusor, prolapse of bladder or bowel, bladder infection, pelvic floor muscle weakness or consuming too much caffeine.
- Urge incontinence is also associated with neurological conditions (Parkinson’s disease, MS, Stroke) along with deconditioned voiding, poor toileting habits, abdominal/pelvic surgeries, constipation and straining.
What Is Bowel Dysfunction?
- Obstructed bowel motion due to over-stretched pelvic floor support structures (descending perineal syndrome), stool caught in rectum or inhibition due to pain postnatally or post-operatively
- Faecal incontinence due to incompetent pelvic floor muscles or stool consistency too loose.
- Medical and Pain syndromes e.g. Crohn’s Disease
What Should I Do If I Have Incontinence?
Don’t put up with it! Do something about it!
Discuss your concerns with a Health Professional trained specifically in the area of Incontinence (Continence and Pelvic Floor Physiotherapist) or your GP A multifaceted approach is needed: incontinence can be managed and prevented by adopting healthy diet and lifestyle habits combined with addressing specific individual needs identified by Health Professionals.
What To Expect With A Pelvic Floor Physiotherapy Consultation?
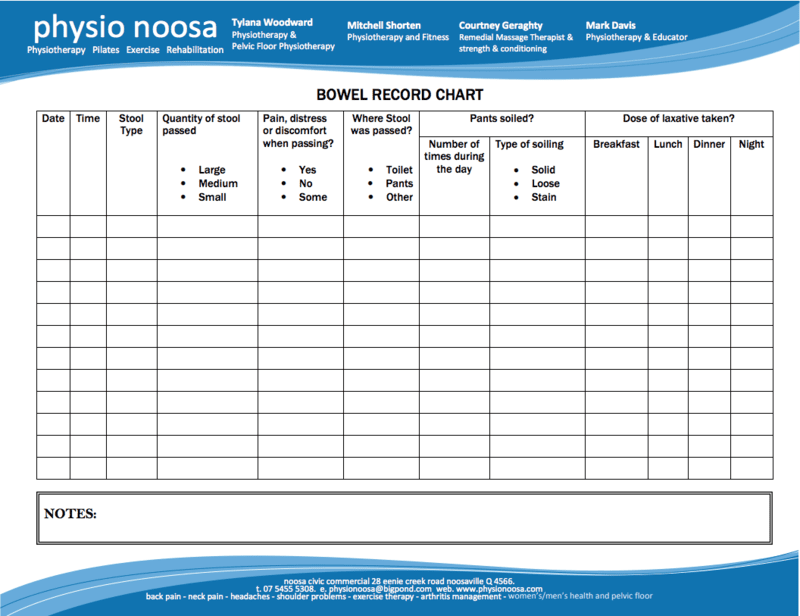
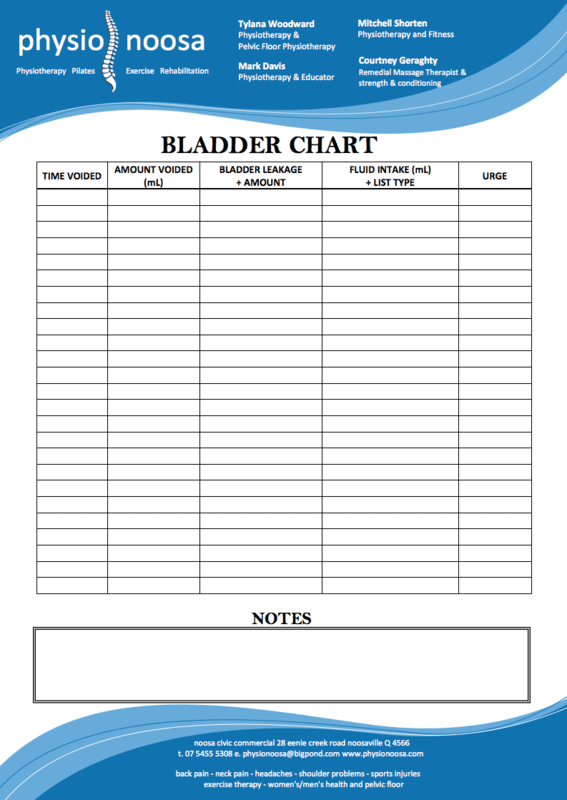
- Discuss your problems and other relevant health information. Charting your bladder and bowel habits can be useful to collect data to identify patterns and problems.
- You’ll have an examination of your pelvis, abdomen, pelvic floor muscles, bladder and pelvic organs with a real-time ultrasound machine. At least a half full bladder is needed to allow for visualising of the structures in the pelvis. Assessment of the pelvic floor muscles is undertaken using the ultrasound so there is often no need to do an internal examination. If an internal examination is recommended, it will be discussed with your Pelvic Floor Physiotherapist.
- THERE WILL BE EXERCISES TO DO!! Expect this! Prepare for this! Commit to the program! Nothing in this world happens with the wave of a magic wand!
- You will be taught how to do your Pelvic Floor Exercises whilst having an ultrasound scan done. A specific program will be drawn up for you based on the results of the scan. We are all individual and need to be treated as such.
- Follow up appointments with repeat scanning will need to be done at intervals to assess improvements and upgrade your individual program.
- As with any training program, there will be good days and bad days. Some days leakage may be better and some days it may be worse. Stick with it and things will improve or even completely disappear with diligence and commitment!
- Lifestyle improvements specific to your needs will also be discussed. This may include diet, soluble fibre intake, exercise, fluid intake, general health improvements, toileting habits and cessation of causative factors
Forms
Men's And Women's Health Resources
About Us
If you are suffering from back, neck, knee, ankle or shoulder pain, require post-operative rehabilitation or simply want to improve your fitness, Physio Noosa can help you. Our expert team of physiotherapists provide a range of services to assist in managing your condition, dry needling, exercise therapy, physiotherapy and even Pilates.
Physio Noosa. All Rights Reserved.
Contact Us
To book an appointment with one of our experienced therapists, or for more information, please contact us.
Phone: 07 5455 5308
Email: physionoosa@bigpond.com